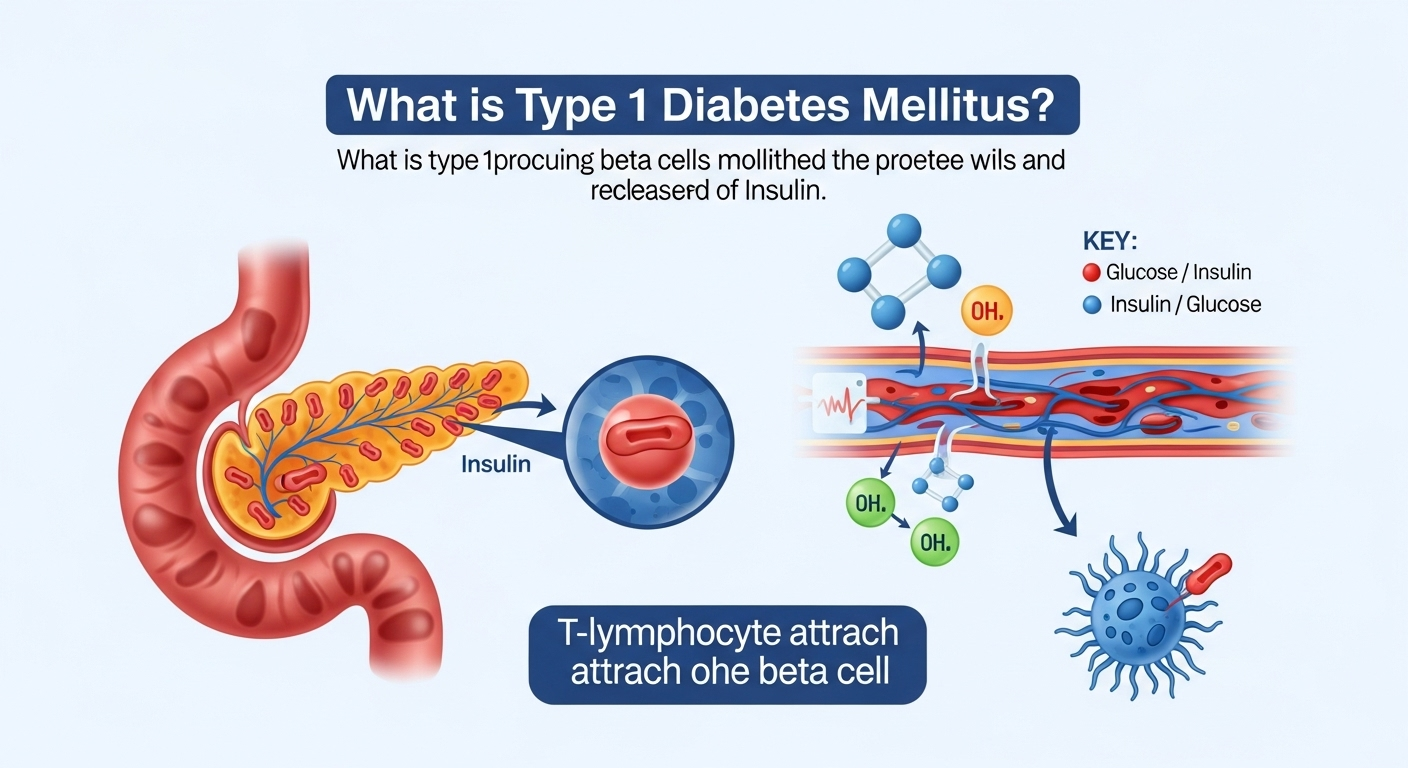
Type 1 diabetes mellitus (often just called Type 1 diabetes) is a chronic condition that occurs when the body’s immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. This results in little to no insulin production, which is essential for regulating blood sugar (glucose) levels. As a result, people with Type 1 diabetes must carefully manage their blood sugar levels throughout their lives.
In this article, we’ll take a closer look at what Type 1 diabetes is, its causes, symptoms, treatment, and how it can be managed.
What Is Insulin and Why Is It Important?
Before diving into Type 1 diabetes, it’s essential to understand what insulin is and why it’s important. Insulin is a hormone produced by the pancreas, a small organ located behind the stomach. It helps regulate blood sugar levels by allowing glucose to enter the body’s cells, where it is used for energy. Without enough insulin, blood sugar levels can rise to dangerously high levels, leading to serious health problems.
What Causes Type 1 Diabetes?
Type 1 diabetes is primarily caused by an autoimmune reaction. This means the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. The exact reason why this happens is not fully understood, but it is believed to involve a combination of genetic and environmental factors.
- Genetics: Certain genes can make someone more susceptible to Type 1 diabetes. If you have a family history of Type 1 diabetes, your risk of developing it is higher, but many people with Type 1 diabetes don’t have a family history.
- Autoimmune Response: In Type 1 diabetes, the immune system targets the pancreas’s beta cells, which are responsible for producing insulin. Over time, this leads to insulin deficiency.
- Environmental Triggers: In some cases, an infection or other environmental factors may trigger the immune response that causes Type 1 diabetes. However, these triggers are not fully understood and can vary from person to person.
Symptoms of Type 1 Diabetes
The symptoms of Type 1 diabetes often develop quickly and can be severe. Common signs include:
- Increased thirst (polydipsia)
- Frequent urination (polyuria)
- Extreme hunger (polyphagia)
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow-healing sores or infections
- Nausea or vomiting (especially in extreme cases)
These symptoms occur because without enough insulin, the body cannot properly use glucose for energy, leading to high blood sugar levels and dehydration.
How Is Type 1 Diabetes Diagnosed?
Diagnosing Type 1 diabetes typically involves a combination of physical exams, medical history, and blood tests. The tests used to diagnose Type 1 diabetes include:
- Fasting Blood Sugar Test: This test measures blood sugar levels after you have fasted overnight. A result of 126 mg/dL (milligrams per deciliter) or higher may indicate diabetes.
- Oral Glucose Tolerance Test: This test checks how your body processes sugar. After drinking a sugary solution, your blood sugar is tested at different intervals to see how your body responds.
- Hemoglobin A1C Test: This test measures your average blood sugar levels over the past 2 to 3 months. An A1C level of 6.5% or higher may indicate diabetes.
- Urine Test: This test can check for the presence of ketones or excess sugar in the urine, both of which can be signs of uncontrolled Type 1 diabetes.
- C-Peptide Test: This test can assess how much insulin the body is producing, and a low level suggests Type 1 diabetes.
Treatment of Type 1 Diabetes
Since Type 1 diabetes is an insulin deficiency disorder, the primary treatment is insulin therapy. Unlike Type 2 diabetes, which is often managed with oral medications, people with Type 1 diabetes need insulin injections or an insulin pump to regulate their blood sugar levels.
Types of Insulin
There are several types of insulin used to treat Type 1 diabetes. They vary in how quickly they work and how long they last:
- Rapid-acting insulin: This insulin starts working within 15 minutes and lasts for 3-5 hours. It’s typically used before meals to manage the rise in blood sugar from food.
- Short-acting insulin: This insulin begins to work within 30 minutes and lasts for about 6-8 hours.
- Intermediate-acting insulin: This insulin takes about 2-4 hours to start working and lasts for 12-18 hours.
- Long-acting insulin: This insulin works gradually over 24 hours to maintain consistent blood sugar levels.
Insulin Delivery Methods
Insulin can be delivered through various methods, including:
- Insulin Injections: The most common method, using a syringe or insulin pen to inject insulin into the body.
- Insulin Pumps: Small devices worn on the body that deliver continuous insulin through a catheter placed under the skin.
- Insulin Inhalers: Less common, but some people use inhaled insulin during meals to manage blood sugar.
Continuous Glucose Monitors (CGM)
A continuous glucose monitor (CGM) is a device that provides real-time blood sugar readings throughout the day and night. This helps people with Type 1 diabetes monitor their blood sugar levels and make adjustments to their insulin doses as needed. CGMs can be a useful tool for managing the condition and preventing complications.
Lifestyle Changes for Managing Type 1 Diabetes
In addition to insulin therapy, making certain lifestyle changes can help manage Type 1 diabetes:
1. Healthy Eating:
A balanced diet with a focus on whole grains, vegetables, lean proteins, and healthy fats can help regulate blood sugar levels. It’s essential to count carbohydrates and be mindful of the glycemic index of foods, as carbs directly affect blood sugar levels.
2. Exercise:
Physical activity helps regulate blood sugar by increasing insulin sensitivity. Aim for at least 150 minutes of moderate-intensity exercise per week, such as walking, swimming, or cycling. However, it’s important to monitor blood sugar levels before, during, and after exercise.
3. Stress Management:
Stress can cause blood sugar levels to rise, so practicing stress-reduction techniques like deep breathing, yoga, and meditation can be beneficial.
4. Regular Monitoring:
People with Type 1 diabetes must check their blood sugar levels regularly, typically several times a day, to ensure they are in the target range. This helps prevent both high and low blood sugar levels, which can lead to complications.
Long-Term Complications of Type 1 Diabetes
If Type 1 diabetes is not managed properly, it can lead to long-term complications, such as:
- Heart disease: Increased risk of heart attacks, strokes, and other cardiovascular problems.
- Nerve damage (neuropathy): This can lead to tingling, numbness, and pain, particularly in the feet and hands.
- Kidney damage (nephropathy): Damage to the kidneys can lead to kidney failure and may require dialysis or a kidney transplant.
- Eye damage (retinopathy): Diabetes can damage blood vessels in the eyes, leading to vision problems or blindness.
- Poor circulation: Can result in slow-healing wounds and infections, especially in the feet.
FAQ About Type 1 Diabetes
Q: Can Type 1 diabetes be prevented?
A: No, Type 1 diabetes cannot be prevented. It is an autoimmune condition that develops due to a combination of genetic and environmental factors.
Q: Is Type 1 diabetes the same as Type 2 diabetes?
A: No, Type 1 diabetes is an autoimmune condition where the body stops producing insulin, while Type 2 diabetes is primarily caused by insulin resistance and is more common in adults.
Q: Can people with Type 1 diabetes live normal lives?
A: Yes, with proper management of insulin, diet, exercise, and blood sugar levels, people with Type 1 diabetes can live full and healthy lives.